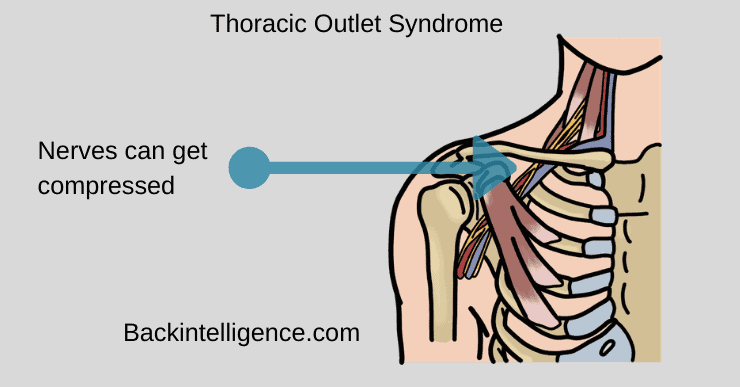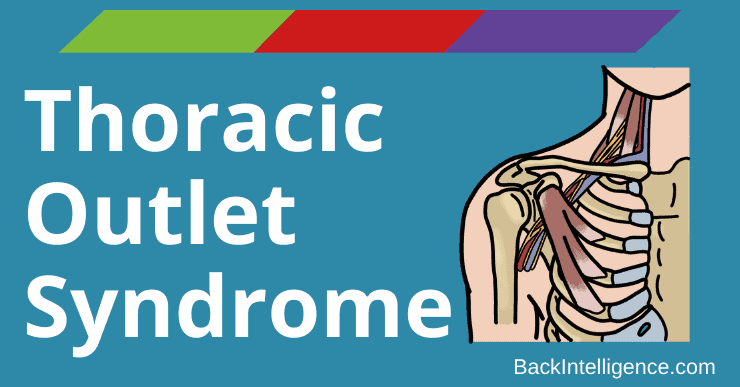
Thoracic Outlet Syndrome (TOS) is a diagnosis of omission meaning physicians rule out all other conditions first. It happens when nerves that run from the base of the neck down the arm get compressed. The nerves that get compressed are a bundle of nerves called the brachial plexus.
The thoracic outlet is located above the first rib and underneath the clavicle (collarbone).[1] It contains three spaces that house important nerves called the brachial plexus and blood vessels including the subclavian nerve and artery. Compression of these structures is what causes the symptoms related to TOS.[2]
TOS can occur in just one side of the body or on both sides.
There are three subtypes of thoracic outlet syndrome including neurogenic TOS, arterial TOS and vascular TOS. Neurogenic Thoracic Outlet Syndrome is the most popular type consisting of 95% of total cases so we will focus the rest of the article on Neurogenic TOS.
TOS is most common in women between the ages 20-50 years old although other age groups and men could also have this condition.[3]
Similar conditions that need to be ruled out are problems with the cervical (upper part below base of skull) spine, and shoulder dysfunction.[4] If you have widespread symptoms or pain going down the arm that is changed depending on arm, neck or shoulder position you should first diagnose cervical spine problems or shoulder dysfunction, before assuming it’s TOS.[4]
What is the Cause?
- Having a history of neck trauma from an auto accident or repetitive motions may cause TOS symptoms in people that are predisposed based on variations in their bodies.[1]
- Repetitive motions could cause it from occupations such as electrician or hairdresser, or hobbies such as swimming, playing baseball or playing an instrument.[1]
- Variation in where the scalene muscle connects to the ribs can cause compression of the brachial plexus nerves or the subclavian artery in the interscalene triangle.[4]
- An extra muscle called the scalenus minimus that is not present in a most people, may be present in 30-50% of TOS cases.[4]
- Hypertrophy (increased size) of the muscle from overuse or repetitive movements can cause compression.[2][4]
- Presence of a cervical rib fused to the first rib occurs in less than 1% of the overall population and they are usually asymptomatic, but can become symptomatic after neck trauma and cause TOS.[1][4]
- Abnormal movement of the acromioclavicular (AC) joint or sternoclavicular (SC) joint following injury could also cause TOS.[4]
How to tell if you have TOS?
A doctor could formally diagnose TOS by giving you a physical exam, asking questions about how long you’ve had the symptoms and activities that make the symptoms better or worse, but there is a lot you can look for on your own. If you have TOS you may experience pain or numbness/tingling in the opposite side of your body while rotating your head to the side (as if saying no) or looking up to the ceiling meaning you may have pain in your right side when rotating your head to the left or vice versa. If you have neck or arm symptoms (either pain or numbness/tingling) and they change based on the position of your neck you may have TOS.[4]
While speaking to the clinician you will be asked about when symptoms began, and activities that make it better or worse. The clinician will look to see if movement of the neck causes pain, will look at your overall posture, and may use certain movement tests in order to provoke the pain.[4]
An MRI could be used to look at what area is compressed, but it is not necessary to benefit from treatment.[5]
Symptoms:
- “Achy” Pain that travels from the neck and shoulder down the arm[4]
- Numbness and tingling[1][4]
- Weakness is less common
- Vasomotor changes in arm (symptoms due to constriction and dilation of blood vessels)[4]
- Arm heaviness especially with overhead activities[4]
- Noticeable muscle wasting[2]
- Pale and cool hands[1][4]
- Forward head posture due to pec tightness[6]
- Occipital headaches[1]
The symptoms listed above may be present during your everyday activities as well as during sleep. Shoulder, arm and hand heaviness is especially common during above-the-shoulder activities. Symptoms may also develop weeks after the trauma was experienced rather than immediately after.[4]
We are going to dive into the exercises below. Please note, it is best to try exercises and stretches first, but for any patient with neurogenic TOS that has failed to respond to nonsurgical management, surgical intervention is warranted.[4]
The Complete Posture Fix (With Dr. Oliver)
Fix your Rounded shoulders & Fwd Head posture, get out of pain and increase your mobility.
Learn More
Exercises For Thoracic Outlet Syndrome
Below are 5 exercises that can be used to help manage symptoms of thoracic outlet syndrome. Along with the following exercises you should work on improving posture/workplace setup to allow for better positioning of shoulders, muscle relaxation and reducing repetitive movements.[4][6]
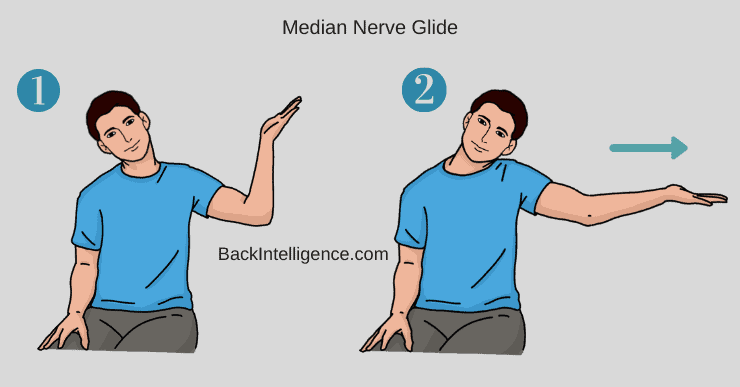
Exercise #1: Median Nerve Gliding[4]
This is a Nerve glide, and can provide some relief. If it doesn’t, please stop and try a different exercise below.
- Stand upright and place symptomatic arm out to the side with elbow bent to 90 degrees with palm flat and fingers facing away from you, as if pretending to be a waiter carrying a tray with head tilted towards non-symptomatic side (as if putting your ear on your shoulder)
- Tilt head towards symptomatic side (as if putting ear on shoulder) at the same time you straighten your elbow.
- Tilt head towards non-symptomatic side again as you return the elbow to a bent position, again as if carrying a tray.
- Repeat 10x. Can be done multiple times a day.
- Should not be painful. If this causes pain, stop doing exercise because it could cause more irritation to the nerve.
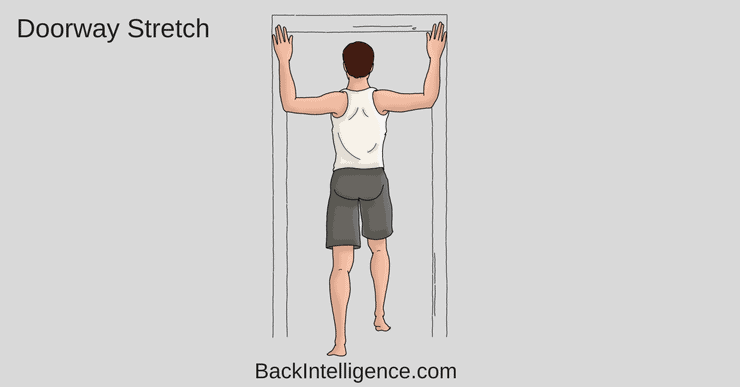
Exercise #2: DoorWay Stretch[6]
This stretch will stretch out your chest and shoulder muscles
- Stand in a doorway and place arms up at shoulder height so arms are touching the door frame.
- Take a step forward through the doorway with one foot until you feel a stretch across the front of your shoulders/chest.
- Hold stretch 20-30 seconds, rest then repeat.
- Your legs will control the amount of stretch you are receiving.
- If this position is uncomfortable you can place your arms below shoulder level) and repeat the stretch.
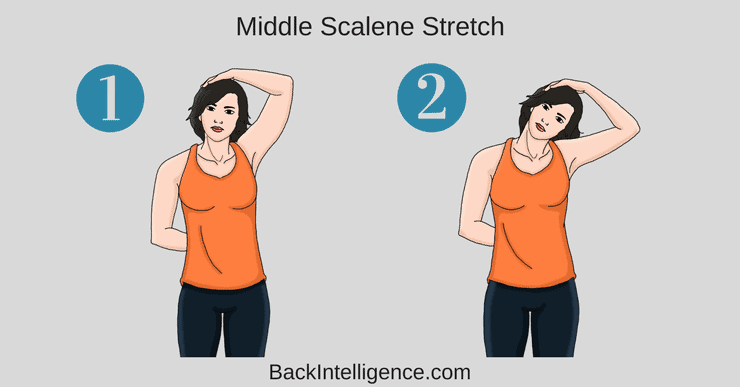
Exercise #3: Middle Scalene Stretch
This will release the Scalene muscle in the neck
- Use one hand (ex. L) to place behind back, and the other hand (ex. R) over your head and place it on the L side of your head.
- Using your Right hand pull your head to the right side, as if bringing your ear to your shoulder.
- Hold stretch for 2x 30 seconds and repeat daily.
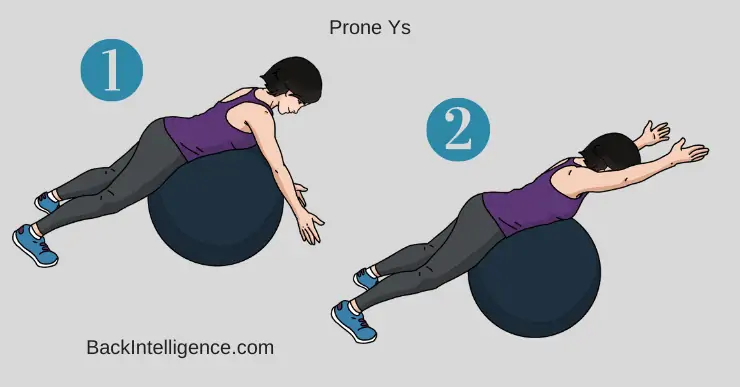
Exercise #4: Prone Y’s[6]
This exercise is done for scapular stabilization and strengthening your back.
- Can be done off the side of a bed or while lying on your stomach on a large exercise ball with arms hanging straight down.
- Raise your arms up to a 45-degree angle (with thumbs up), making a Y between your arms and body. Only raise arms up to shoulder height.
- Now lower arms to starting position
- Build up to 2x 10
** Careful not to arch your low back as you lift your arms.
** Do not shrug your shoulders
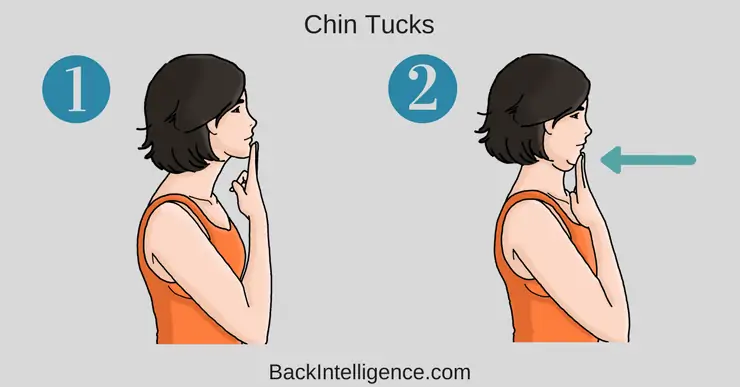
Exercise #5: Chin Tucks
This exercise will activate and strengthen your deep cervical muscles (front of the neck muscles).
- Place 2 fingers at the bottom of your chin.
- Gently tuck your chin in and retract your head backwards. At the same time, use your fingers to keep the chin tucked in the entire time.
- Hold the end position for 3 to 5 seconds.
- Relax your neck for a moment (Let the neck come fwd).
- Aim for 2 to 3 sets of 10 repetitions.
** You should feel like the back of your neck is lengthening or “pulling up”, and there will be packing in front of your neck.
Conservative (nonsurgical) management should be tried first in patients with TOS. Surgery should only be considered with other forms of TOS (arterial/venous) or severe neurogenic TOS where symptoms continue after 6 months of nonsurgical treatment or patient has significant muscle atrophy or is showing severe disability. Appropriate treatment often leads to reduction of symptoms in most patients.[4]
Finally, Check out this video on TOS:
Learn More
Related:
How To Do Chin Tucks Exercise Correctly (Video)
How To Get Rid of Neck Pain (9 Best Neck Stretches & Releases)
Cervical Facet Joint Pain – Treatment & Exercises
Easy Sternocleidomastoid Stretch (SCM) – Posture Correction
Winged Scapula Exercises
Sources:
[1] Sanders RJ, Hammond SL, and Rao NM. Diagnosis of thoracic outlet syndrome. JVS. 2007; 46(3)p.601-604. http://doi.org/10.1016/j.jvs.2007.04.050.
[2] Jones MR, Prabhakar A, Viswanath O et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis and treatment. Pain Ther. 2019; 8: 5-18. http://doi.org/10.1007/ss40122-019-0124-2.
[3] Hwang JH, Ku S, Jeong JH. Traditional medicine treatment for thoracic outlet syndrome: a protocol for systematic review of randomized controlled trials. Medicine 2020;99:27. http://dx.doi.org/10.1097/MD.0000000000021074
Doctor of Physical Therapy and currently works full time as a pediatric physical therapist. Rachel has worked in Sports, Inpatient Rehab and Outpatient Ortho settings under the guidance of incredible mentors focusing on low back pain. Rachel believes in holistic and patient centered care and enjoys developing their course of treatment.