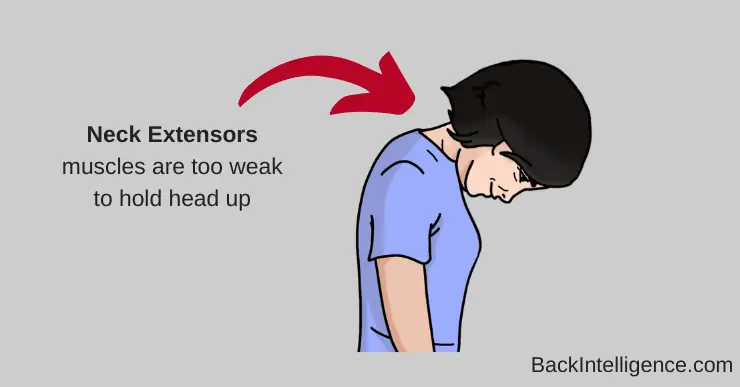
Dropped head syndrome (DHS) is known as a “chin on chest” deformity. It is a rare condition that is due to the gradual weakening of the muscles in the back of the neck, called “Neck Extensors”.[1][2][3]
These Neck Extensor muscles help keep your head upright so you can look at the world in front of you. When these muscles become weak, they are then unable to hold the weight of the head and neck, therefore “dropping” the head forward and down.[1]
Dropped head syndrome typically affects older adults. The mean age range for people who get diagnosed with Dropped Head Syndrome is 63 Years of age.[4]
This neck deformity can be reversed (at least temporarily) by using passive head extension or by lying supine (on the back). [2][3]
Interesting Find: Upon admission a 67-year old man with DHS said he could maintain his head up with extreme effort only for about five minutes.[2]
Dropped Head Syndrome Symptoms
Below are common symptoms of dropped head syndrome. Someone who has DHS may have some OR all of these symptoms:
- Chin to chest position: The head’s natural resting place while sitting or standing is looking downward with the chin on the chest.[1][2][3]
- Severe weakness of the muscles in the back of the neck that are responsible for extending the neck.[1][2][3]
- Can be present with thoracic kyphosis and/or cervical kyphosis[3][6]
- Neck pain[4]
- Tingling in hands[2]
- Disruption in social life[2]
- Trouble eating and difficulties in chewing and swallowing.[2][4]
- Gait abnormalities from not being able to look forward leading to.[5]
Learn More
What Causes Dropped Head Syndrome?
According to a 2019 systematic review, Dropped Head Syndrome cases were due to:[4]
- Isolated neck extensor myopathy, (31.8%)
- Parkinson’s disease (20.2%)
- Myasthenia gravis (12.4%)
- Amyotrophic lateral sclerosis, also known as ALS (7.0%)
Here is a more detailed breakdown of the many conditions that can cause DHS[6]:
Neurological
- Amyotrophic lateral sclerosis (ALS)
- Parkinson’s disease
- Cervical dystonia
- Cervical myelopathy
- Multiple system atropy
- Postpolio syndrome
- Chronic inflammatory polyneuropathy
- Tardive dyskinesia
Neuromuscular
- Myasthenia gravis
- Lambert-Eaton myasthenic syndrome
Muscular
- Polymyositis
- Scleromyositis
- Isolated inflammatory axial myopathy
- Myopathy
- Fascioscapulohumeral dystrophy
- Postradiation neck extensor myopathy
- Anterior scar contracture
- Postbotulinum toxin injection
- Cushing syndrome
- Carnitine deficiency
- Hypothyroidism
- Hypokalemia
- Hyperparathyroidism
Other causes
- Cancer
- Post-surgical
How Can you Treat Dropped Head Syndrome?
While surgery should be the last resort, at present, surgery seems to be the only definitive solution for correction and stabilization of DHS.[5]
As always, before considering surgery, make sure to get several opinions from several doctors.
The 3 ways to treat dropped head syndrome:
Sources:
[1] Burakgazi AZ, Richardson PK, Abu-Rub M. Dropped head syndrome due toneuromuscular disorders: Clinical manifestation and evaluation. Neurol Int. 2019;11(3):8198. Published 2019 Jun 19. doi:10.4081/ni.2019.8198
[2] Rahimizadeh A, Soufiani H, Rahimizadeh S. Cervical Spondylotic Myelopathy Secondary to Dropped Head Syndrome: Report of a Case and Review of the Literature. Case Rep Orthop. 2016;2016:1-7. doi:10.1155/2016/5247102
[3] Taniguchi S, Takahashi H, Aoki Y, et al. Surgical treatment for dropped head syndrome with cervical spondylotic amyotrophy: a case report. BMC Res Notes. 2018;11(1):500. Published 2018 Jul 24. doi:10.1186/s13104-018-3612-2
Received her Doctorate in physical therapy from Rutgers University in 2016. Since graduation she has been working mostly with outpatient orthopedics. She says: “I believe that if you can move freely and pain-free throughout your life, you can live life to it’s fullest. As a Certified Strength and Conditional Specialist and a CrossFit coach, I believe that physical abilities are directly correlated with quality of life.”