Frozen shoulder, also known as adhesive capsulitis, is a thickening of connective tissue in the shoulder joint capsule.[3] It causes pain and loss of range of motion when the arm is moved actively or passively, which can make it difficult to complete daily activities.[1][2]
There is only so much room in the shoulder joint capsule so as it swells, other parts get cramped which causes difficulty with movement.[3] According to this study, “It is likely that limitations in range of motion and the pain associated with frozen shoulder are not only related to capsular and ligamentous tightness, but also fascial restrictions, muscular tightness, and trigger points within the muscles.”
Many people will naturally recover without any form of treatment, but may take a long time and complete range of motion may never recover.[1][2][4]
There are two types of frozen shoulder: primary and secondary. Primary frozen shoulder is idiopathic, but is associated with diabetes or thyroid conditions.[2] Secondary frozen shoulder can be caused by shoulder injuries or immobilization.[2]
Frozen shoulder typically occurs in about 2-5% of people.[1][2][3] It most commonly affects women, rather than men between 40-65 years old.[2][3][4]
Frozen shoulder typically goes through 3 phases and lasts anywhere from 12-36 months though it can vary.
The 3 Phases of Frozen Shoulder:
Stage 1
This is the freezing phase which includes shoulder pain and decreases in range of motion of the shoulder especially in external rotation (rotating the arm out) and abduction (bringing the arm out to the side). [2][4]
Stage 2
This is the frozen phase where the pain decreases, but the stiffness and range of motion progressively increases. [2][4]
Stage 3
This is the thawing phase where motion is gradually restored and pain gets better.
[2][4]
How are Muscles/Joints/Bursa affected?
The rotator cuff muscles keep the shoulder stable during motions and include the supraspinatus, infraspinatus, teres minor and subscapularis. These muscles can become tight/stiff during the 1st stage (Freezing), and need stretching/releasing. Later on during 3rd phase (Thawing) it is important to strengthen these muscles, as they could get weak from underuse.
Related: How To Fix Shoulder Impingement
Symptoms of Frozen Shoulder
- Shoulder pain [2][3][4]
- Shoulder stiffness [2][4]
- Loss of range of motion in a specific pattern called a capsular pattern (external rotation, abduction, flexion, internal rotation) [2][3][4]
- May hike shoulder to attempt to increase range of motion [3]
- Symptoms are typically worse at night [2][4]
- Difficulty completing activities of daily living including lifting arm above head/reaching across body/behind back [2]
- Shoulder muscle weakness [2]
- Forward head posture [3]
- Decreased arm swing during walking
Causes of Frozen Shoulder
Primary cause:
- Idiopathic, meaning it occurs spontaneously without a specific event triggering it. [2][3][4] It is often associated with: Diabetes Mellitus, Thyroid Conditions, Parkinson’s Disease [2].
Secondary cause:
- Caused by shoulder injury
5 Exercises for Frozen Shoulder
Conservative treatment should be tried first, and done for 6 months before surgery is considered.[1]
According to this study: “As little as 4 weeks of targeted intervention can improve pain and strength in frozen shoulder patients”. [4]
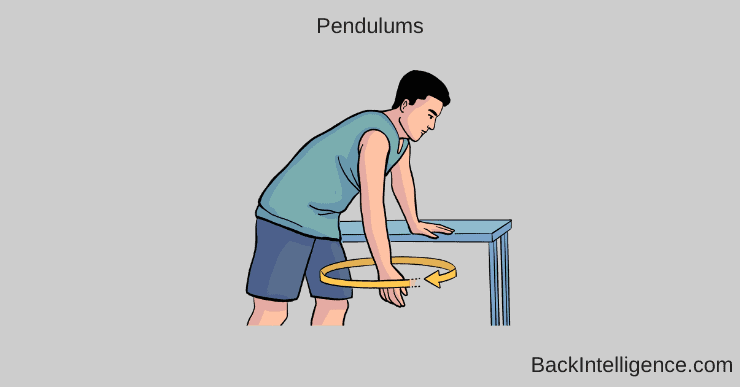
1. Pendulums (ROM)
- Stand up bending forward at the hips and allow your arm to completely relax. It should be hanging down – gravity will help with this to unweight the shoulder joint.
- You can hold onto a table or counter with your opposite hand for added support.
- Rock your body forward and backwards and allow your momentum to swing your arm in a circular motion.
- This should be a passive motion with the momentum moving your arm rather than your muscles.
- Complete 3 x 10 circles going both clockwise and counterclockwise 2x/day
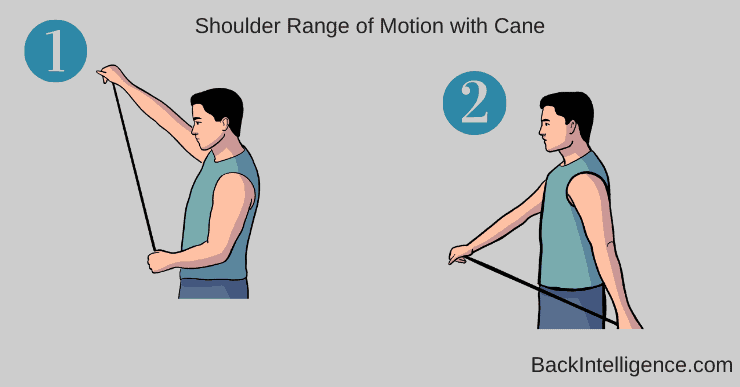
2. Active-Assisted Flexion Range of Motion with Cane
- Stand up while holding a broom in both hands. The hand of the injured shoulder should be placed on the end of the broom.
- Use your non injured side to push the injured arm back as far as you can tolerate without pain. You can assist the motion using muscles on your injured side.
- This motion should be done slowly and in a pain free range of motion
- Complete 2 x 10 reps, 2x/day
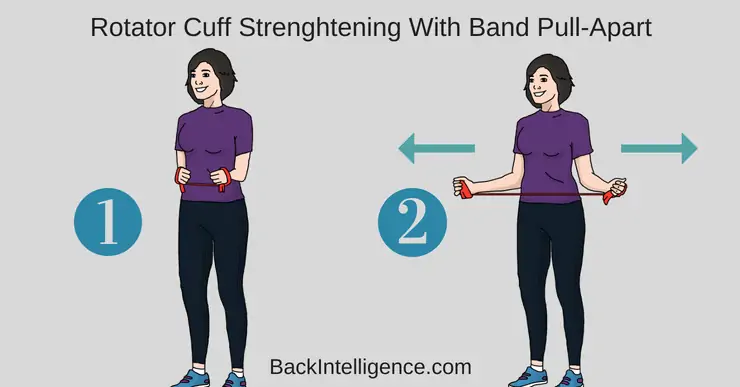
3. External Rotation Isometric Strengthening
- Stand up straight. Bring your arms up to 90 degrees with your elbow by your sides and palms facing upwards.
- Slowly bring your hands away from each other while keeping your shoulders back.
- Focus on squeezing your shoulder blades back and down
- Complete 2 x 10 reps
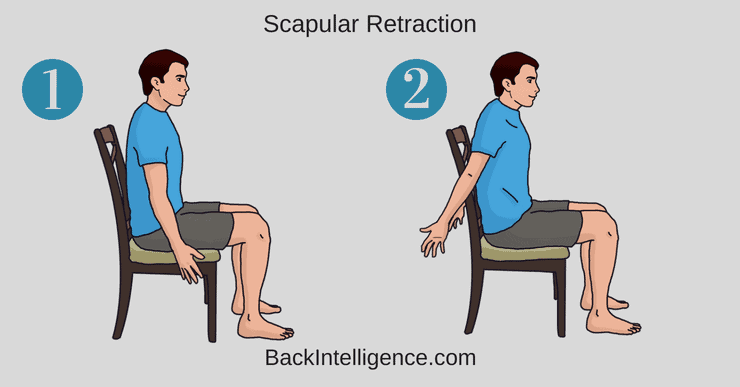
4. Scapular Retractions
- Position your feet and knees slightly wider than your hips, as you sit on a chair.
- Maintain a chin tuck and raise your chest up, allowing your spine to be in a neutral position.
- Rest both of your arms down by your sides.
- Now bring your arms back and externally rotate them so that your thumbs are pointing backwards.
- Hold this position for 5-10 seconds and release.
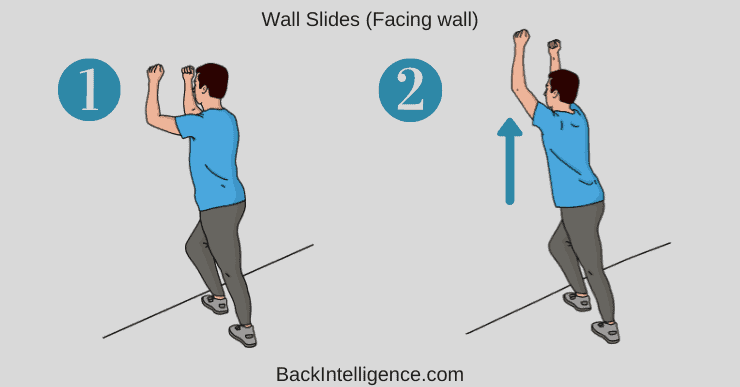
5. Wall Slides
- Position your forearms on the wall with elbows at 90 degrees, one foot in front of the other.
- Now, glide your forearms up the wall (without arching the low back)
- Then glide the forearms down the wall
- Strive for 15 reps, 2 sets.
Besides Exercise, Other Treatment Options Include:
Check Out The Video:
Related:
3 Overhead Shoulder Press Mistakes
3 Self Tests For Shoulder Impingement (Easy To Do)
How To Fix Shoulder Impingement with Exercises
Fix Pain Between Shoulder Blades In Upper Back
Dowager’s Hump Exercises – AKA Hyperkyphosis
Sources:
[1] Cho CH, Bae KC, Kim DH. Treatment strategy for frozen shoulder. Clin Orthop Surg.2019;11:249-257.
[2] Yvonne Chan HB, Pua PY, How How C. Physical therapy in the management of frozen shoulder. Singapore Med J. 2017;58(12):685-689. doi: ¨10.11622/smedj.2017107
[3] Page P, Labbe A. Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther. 2010; 5 (4): 266-273.
Doctor of Physical Therapy and currently works full time as a pediatric physical therapist. Rachel has worked in Sports, Inpatient Rehab and Outpatient Ortho settings under the guidance of incredible mentors focusing on low back pain. Rachel believes in holistic and patient centered care and enjoys developing their course of treatment.